Peripheral T-cell Lymphomas (PTCL) are uncommon, but aggressive forms of non-Hodgkin lymphoma that develop from mature T cells, a type of white blood cell. The most prevalent subtypes include PTCL-NOS (not otherwise specified), AITL (angioimmunoblastic T-cell lymphoma), and ALCL (anaplastic large cell lymphoma). Patients with PTCL are usually treated with a combination of chemotherapy agents, mostly commonly CHOP (cyclophosphamide, adriamycin, vincristine and prednisone). With the exception of a rare variant called ALK-positive ALCL, only about a third of all patients could enjoy long-term disease-free survival, with most patients either having diseases resistant to treatment or recurrent after chemotherapy. As PTCL evolves, it becomes even more molecularly complex due to factors in the tumor microenvironment that make it hard to treat. Ongoing research has been performed in order to try and improve treatment options and increase overall survival for patients with this challenging disease.
To ultimately cripple tumors in patients with PTCL and eradicate the disease from the body, it’s necessary to target the molecular feature of PTCL that helps it grow. Leandro Cerchietti, M.D. Jia Ruan, M.D., Ph.D., and other collaborators from the Lymphoma Program at Weill Cornell Medicine and NewYork-Presbyterian are trying to do just that. New research conducted by the team has shown positive results for this hard-to-treat cancer.
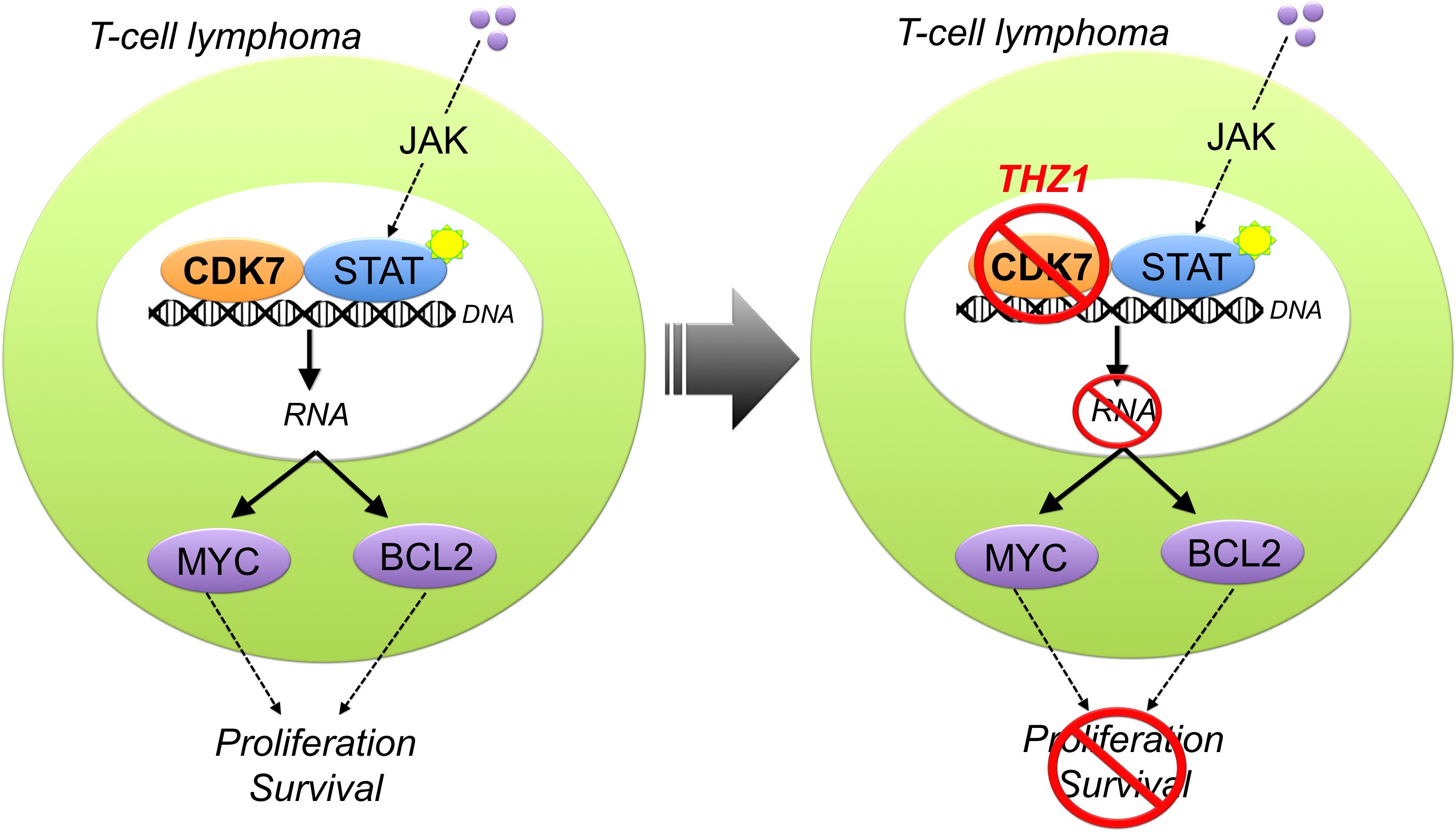
Dr. Cerchietti and his reserach team have discovered that PTCL are sensitive to THZ1, a drug that targets transcription, the first step during gene expression when DNA is copied into RNA. THZ1 was developed by Dr. Nathanael S. Grayand collaborators from the Dana-Farber Cancer Institute. THZ1 works by stopping an enzyme called CDK7 (cyclin-dependent kinase 7) that controls the transcription of lymphoma genes. This interference changes the cells and primes the tumor to better respond to biologic agents, such as BCL2 inhibitors.
For this work, Dr. Cerchietti’s Lab established a collaboration with Drs. Nathanael S. Gray from Dana-Farber and Graciela Cremaschi from the Institute for Biomedical Research and the National Research Council of Argentina. After testing more than 120 FDA-approved compounds and new biologic agents from the Developmental Therapeutics Program, Division of Cancer Treatment and Diagnosis, National Cancer Institute, National Institutes of Health and the Meyer Cancer Center Pre-Clinical Oncology Pharmacy, the investigators found that PTCL are susceptible to inhibitors of the proteasome, epigenetic drugs and compounds that target transcription, like THZ1.
According to Cerchietti, they decided to focus on THZ1 since it demonstrated pre-clinical activity against PTCLs harboring the hard-to-target mutation STAT3. STAT can drive T-cell lymphomas and other tumors when activated by extracellular signaling that involves the phosphorylation of intermediate proteins like JAK. Although inhibitors of JAK proteins have been developed, they are though to be inactive in tumors harboring the STAT3 mutation that does not require the activity of JAK. STAT proteins drive tumors by inducing the transcription of oncogenes like MYC and BCL2. Since this process requires CDK7, THZ1 can decrease the activity of STAT and the production of BCL2 and other proteins.
“Growing scientific evidence supports CDK7 inhibition as a treatment approach for cancers that are dependent on a high and constant level of transcription,” said Dr. Cerchietti. “Targeting CDK7 with THZ1 offers a way to circumvent the aggressive pathway responsible for tumor growth in many cancers, but particularly T-cell lymphomas which respond more positively to BCL2 inhibitors.”
BCL2 inhibitors are a class of drugs that are being tested to treat a variety of blood cancers. Venetoclax is an FDA-approved BCL2 inhibitor that is used to treat chronic lymphocytic leukemia (CLL) with a specific mutation.
“We are excited about these research results and the potential to bring a new treatment to patients with this aggressive lymphoma who otherwise have very few options if their cancer does not respond to chemotherapy,” said Dr. Ruan who leads the T-cell lymphoma clinical program at Weill Cornell Medicine and NewYork-Presbyterian.
“We aim to create transformative medicines that control the expression of disease-driving genes and believe this treatment can provide a profound and durable benefit for patients with a range of aggressive and difficult-to-treat solid tumors and blood cancers,” Nancy Simonian, M.D., CEO of Syros, the pharmaceutical company that is developing the THZ1 compound for clinical trials.
According to Syros, a phase I clinical trial built on this research is slated to open later this year to test the dosing and safety in people with solid tumors and hematological malignancies.
The bulk of this work was supported by the Leukemia and Lymphoma Society through a Translational Research Program awarded to Dr. Cerchietti.
Additional Weill Cornell Medicine contributors to this research include: Florencia Cayrol, Pannee Praditsuktavorn, Tharu Fernando, Rossella Marullo, Nieves Calvo-Vidal, Jude Phillip, Benet Pera, ShaoNing Yang, Kaipol Takpradit, Lidia Romna, Marcello Gaudiano, Ramona Crescenzo and Giorgio Inghirami.
Author: Lindsey Gruenberg (WCM)

